It can happen unexpectedly: A severe back pain, which may radiate into your arms or legs, accompanied by sensory disturbances such as tingling or numbness in your fingers and toes. Sometimes the pain is even accompanied by symptoms of paralysis. Diagnosis? Unfortunately, often a herniated disc.
Disc herniation is a serious disease of the spine that affects around 5% of all people at least once in their lives, according to Inselspital Bern. In some cases, the herniated disc can resolve on its own or with conservative treatment such as physiotherapy, but in other cases, surgery may be necessary to relieve the pain and restore mobility. This is particularly true if the nerve root is affected.
If you are also experiencing severe pain in the spine, we strongly recommend a medical examination to rule out a herniated disc or to determine a suitable treatment method. Find out everything you need to know about the topic here, from symptoms and causes to innovative treatment approaches!
What is a herniated disc?
To explain exactly what a “slipped” disc (technically known as a disc hernia or disc prolapse) is, we first need to take a brief detour into anatomy:
The human spine consists of a series of vertebrae, separated by flexible structures called intervertebral discs. These discs act as shock absorbers and enable movements such as bending, twisting and flexing. They distribute the pressure that is exerted on our spine every day - and this pressure is omnipresent due to lifting heavy objects, sitting for hours on end at the office, unsuitable mattresses, lack of exercise or poor posture. The spine and intervertebral discs wear out over the course of a lifetime, and this natural aging process increases the risk of disc herniation.
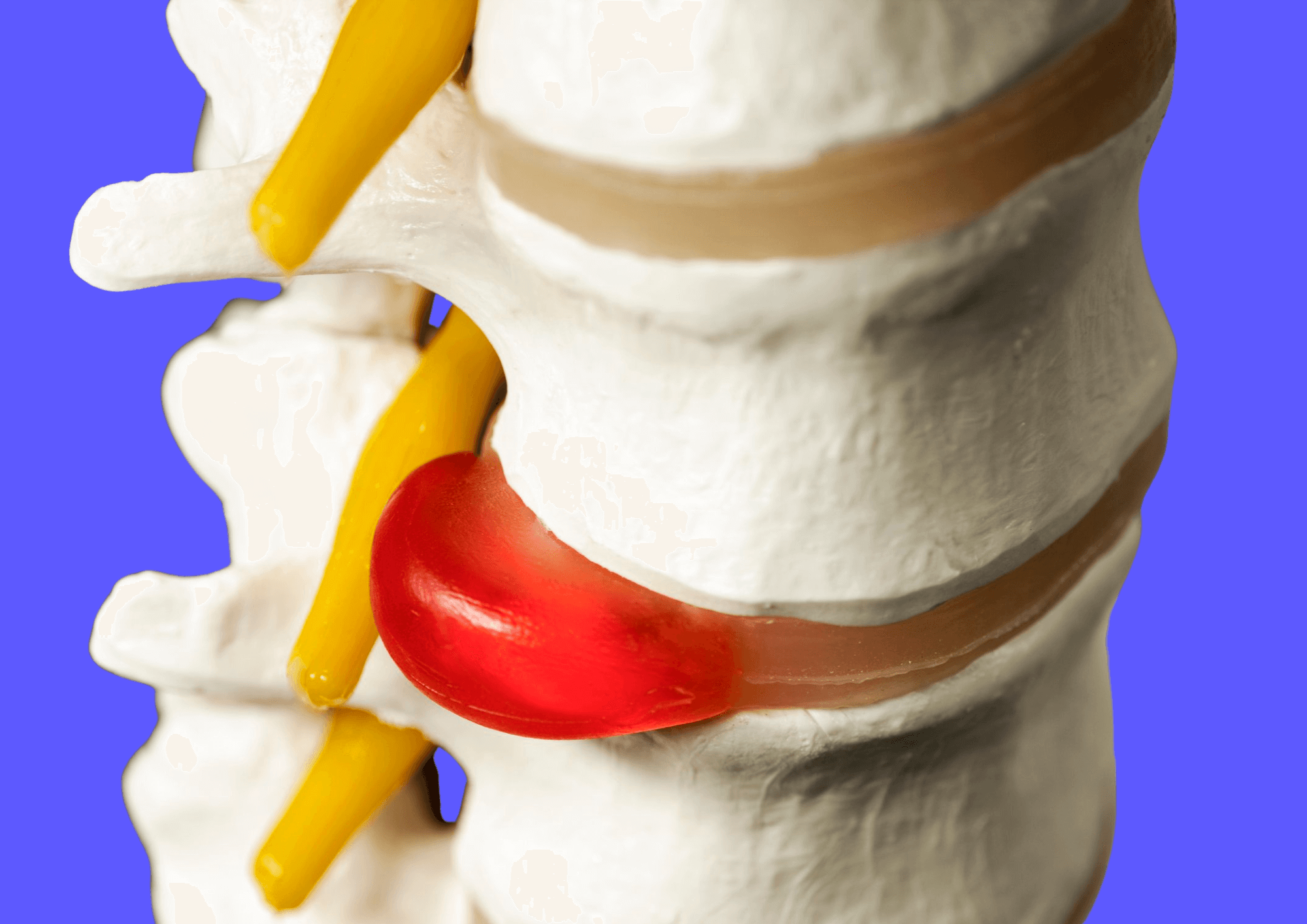
In the event of a herniated disc, the soft, gel-like core of the disc protrudes through its outer fibrous ring and shifts into the spinal nerve canal. The resulting pressure on the surrounding nerve roots can lead to severe pain, numbness, paralysis and limited mobility.
The preliminary stage of a herniated disc: a bulging disc
In medicine, a distinction is made between a herniated disc and a bulging disc, which is the precursor to a herniated disc, so to speak.
While the fibrous ring of a herniated disc is torn by the emerging gelatinous nucleus of the disc, the fibrous ring remains intact in a prolapsed disc (protrusion) and only a bulge or protrusion occurs.
In both forms of the disease, the disc tissue presses on the spinal nerves, which is very uncomfortable for the person affected. The difference between prolapse and protrusion lies primarily in the prognosis: the prognosis for a bulging disc is generally much better than for a herniated disc. This is because the bulging disc can completely regress, whereas the prolapse cannot be reversed completely.
Causes and contributing factors of a herniated disc
- Age-related wear and tear of the intervertebral discs. The disease often occurs between the ages of 30 and 50.
- Chronic overloading of the spine due to heavy physical work or lifting heavy objects with an unfavorable posture.
- Unhealthy lifestyle with an unbalanced diet, lack of exercise and severe obesity.
- Gender - according to an article from the Hirslanden Clinic, men are affected almost twice as often as women.

Typical symptoms of a herniated disc
The symptoms of a herniated disc can vary depending on the location and severity of the affected disc. It does not always have to cause symptoms; a small herniated or bulging disc can remain undetected for a long time.
A herniated disc can occur in any part of the spine, but the lumbar spine is by far the most commonly affected area. The so-called lumbar herniated disc accounts for 90% of all herniated discs. The remaining 10% affect the cervical spine and thoracic spine
The most common symptoms include
- Severe back pain
A typical symptom of a herniated disc is severe - often almost unbearable - back pain, which worsens with sudden movements such as coughing or sneezing. Inactivity and prolonged sitting also increase the pain. - Radiating pain
Although the pain originates in the back, it often radiates to the extremities. And this is where the location of the herniated disc plays a role: if it is in the cervical or thoracic spine, the pain radiates to the arms and fingertips, and neck pain also occurs. If the lumbar spine is affected, the pain can radiate to the legs and feet. - Radiculopathy
Radiculopathy describes the damage or irritation of a nerve root of the spinal cord, which is often the case with a herniated disc. Depending on which nerve root is affected, pain or neurological deficits such as sensory disturbances, numbness or tingling may occur. - Muscle weakness and a feeling of instability
A herniated disc in the lumbar vertebrae often causes a feeling of instability due to muscle weakness in the legs. This can also make it difficult to stand, walk or lift objects. - Symptoms of paralysis and impaired bladder or bowel function
In some cases, a herniated disc can also lead to serious complications, such as paralysis and impaired bladder or bowel control (cauda equina syndrome), which requires immediate medical intervention.

Diagnosis and treatment options
The diagnosis of a herniated disc usually begins with a thorough medical history and physical examination by an orthopedic surgeon. Imaging procedures such as an X-ray, magnetic resonance imaging (MRI) or computer tomography (CT) can help to determine the exact condition of the discs and the location of the herniation. In addition, a neurological examination can be used to draw conclusions about which nerves are irritated or compressed by the herniation.
The treatment of a herniated disc depends on the severity of the symptoms and the region affected. In most cases - approx. 80% according to the University Hospital Zurich - herniated discs heal without surgery. Conservative therapies with anti-inflammatory painkillers, targeted physiotherapy and health-promoting exercise significantly support healing.
If conservative measures are not sufficient, if there is a risk of the pain becoming chronic or in particularly severe cases (e.g. if there is a risk of paralysis), surgery is necessary to relieve the pressure on the nerves and stabilize the affected structures. Minimally invasive surgical procedures such as endoscopic disc surgery can be considered in this case.

The importance of exercise: Back therapy with Akina
Whereas in the past the emphasis was on rest and taking it easy, today's doctors are aware that health-promoting exercise and physiotherapy are crucial in the conservative treatment of herniated discs. The muscles around the spine are strengthened, tension is relieved and pain-related postures are corrected. In addition, mobility and functionality are improved, which, alongside pain relief, has a further significant impact on the quality of life of those affected.
Movement is not only crucial for treatment, but also for the prevention of slipped discs - so it's all the more important to stay active, even if it has already happened!
And this is exactly where Akina comes in. Our AI-based training software with scientifically proven therapy plans helps you recover from or prevent herniated disc.
Our interactive software recognizes your movements via your laptop's camera and gives you valuable feedback in real time. Your physiotherapist can track your progress and deficits via our platform and give you additional tips to make your training even more effective. But that's not all: you can indicate your pain level after each training session - these changes in your perception are recorded and the training intensity can be further adapted to you. We are aware that not only the body but also the mind plays an important role in treatment. That's why our training program is supplemented by stress-reducing mindfulness meditations and interesting educational content about physical and mental health.




